ROI Analysis- The Economics of Prevention
Background
The economics of prevention and the case for readmissions
The cost of healthcare in the US continues to rise to unsustainable levels. Some of this growth is the result of new treatments and innovations, but much of the cost is due to inefficiency and a lack of proactive care. There is a continued emphasis within the healthcare system on preventing the acute onset of many common chronic conditions, including musculoskeletal conditions, heart disease, lung disease, and diabetes. The cost of treating chronic conditions is $3 trillion affecting the lives of millions, the viability of the organizations that fund the cost of healthcare, and ultimately the health of the nation[1-2]. Direct savings for the system can be found in heart attack prevention, early diagnosis of diabetes and the reduced need for procedures such as coronary artery bypasses and total joint replacements – procedures that are both expensive and require extensive medical therapy.
As part of US healthcare reform, reducing hospital readmissions is a key strategy for improving care, increasing quality, and lowering costs. This is known as the Triple Aim[3]. In 2012 the Centers for Medicare and Medicaid Services (CMS) implemented the Hospital Readmission Reduction Program by penalizing hospitals for excessive 30-day readmission rates[4]. Despite this, there have only been minimal decreases in 30-day readmission rates (especially concerning heart failure), leading many hospitals to incur significant financial penalties. More alarmingly, some strategies for reducing readmission rates by decreasing access to healthcare services have led to an increase in mortality rates.
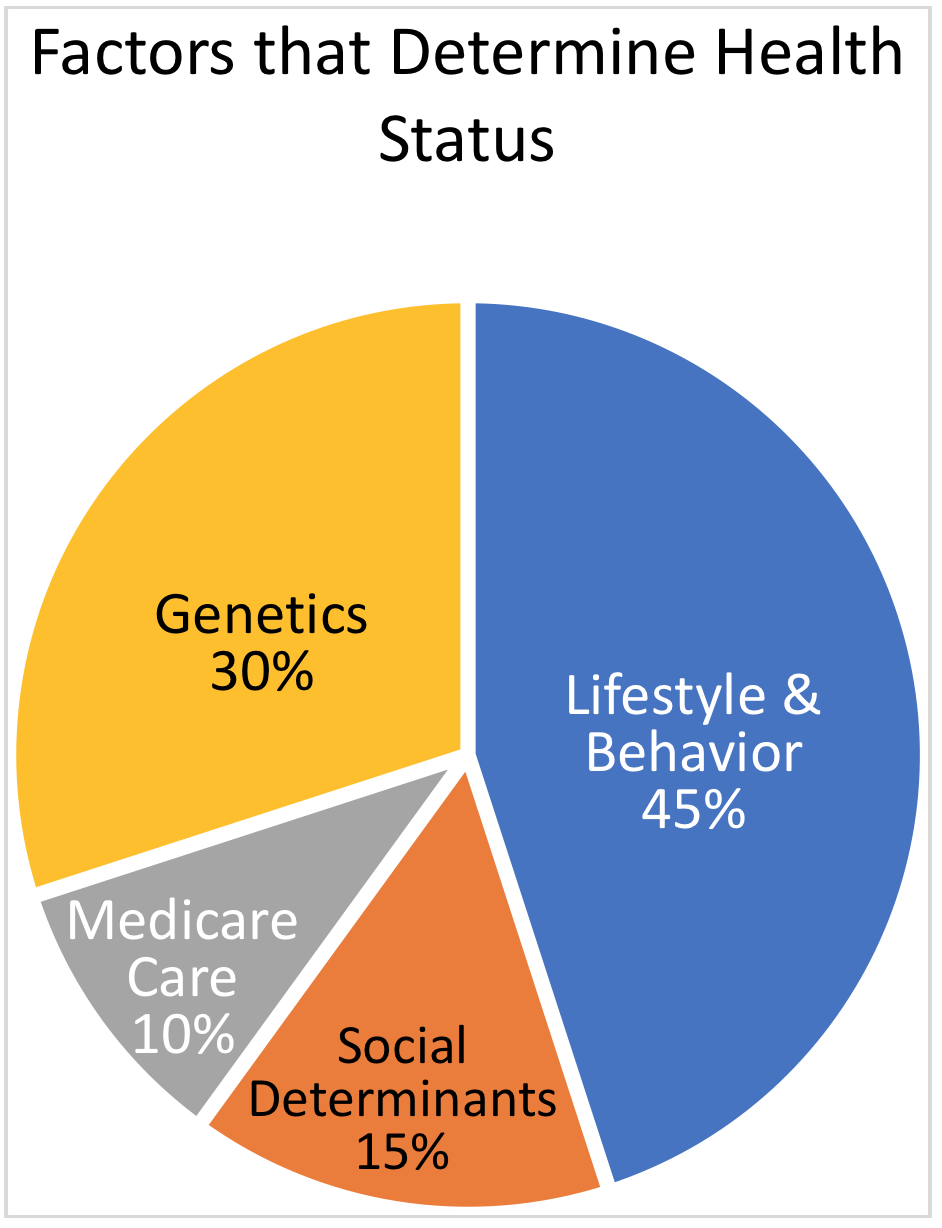
So how are readmissions prevented? By addressing the root cause: the factors outside the healthcare setting that impact patient health. These include healthy lifestyle choices, behavioral factors, social determinants, genetics, and preventive medical care[5]. Rather than restricting access to care, HealthCall focuses on these factors via a novel method of coaching, educating, and assessing within care teams. Patients are assigned to a disease-specific Care Program – such as a heart health or respiratory program – within the HealthCall system. Next, patient-specific care teams are created within HealthCall to extend and coordinate care outside of the healthcare setting. These care teams may be composed of physicians, providers, nurses, caregivers, behavioral health specialists, social services workers, and others. Finally, health assessments and remote patient monitoring is conducted through the patented Automated Patient Response system (HealthCall APR™).
HealthCall APR™ assessments automate routine patient interactions while educating and encouraging patients towards healthier self-care. Best practices include remote monitoring of key biometrics, such as weight, blood pressure and glucose, and key self-care behaviors, such as medication adherence, proper nutrition, physical activity and reporting of symptoms. Meanwhile, responses that are predictive of readmissions and poor health outcomes are identified before the event occurs, resulting in savings for the clinic.
HealthCall APR™ has the advantage of reaching large numbers of patients in an unobtrusive manner, leveraging the use of scarce medical resources and personnel. Using a manage-by-exception model, information can be escalated to the physician quickly, resulting in an intervention or adjustment to the patient’s plan of care. This might include a follow-up phone call, a trip to the physician’s office, or a visit to the emergency department. Early identification of an issue will usually result in a lower cost experience, even if the patient is readmitted to the hospital.
In addition to more proactive clinical care, HealthCall provides a platform to deliver a patient-centered plan of care directly to the patient, significantly improving communication between the patient and their care team members. HealthCall provides self-care tips regarding navigation of the healthcare system, better communication, and shared decision making in a format the patient easily understands[6]. This promotes increased awareness and knowledge of how to live with their condition, a better understanding of what information to pay attention to and, ultimately, a much higher quality of life.
Case Study
This case study is based on a nonprofit health system with more than 200 sites of care based in the Midwest, including one of the largest home health agencies in its state. This home health agency monitors in-network patients with heart failure, COPD, diabetes, or joint replacement. Their goal is to help ensure the successful transition from the hospital to the home, reduce 30-day readmission rates and reduce cost.
The previous system used to monitor patients was rigid, non-customizable, and could not scale with increasing demand, resulting in a process that was lengthy, costly, and frustrating. To meet this need and allow for significant expansion, the home health agency began using HealthCall in September 2016. Managers and nurses from the home health agency met with HealthCall’s implementation team to develop customized, evidence-based care plans tailored to the home health agency’s needs.
HealthCall was selected for its user-friendly, patient-centered, and evidence-based approach to remote patient monitoring. Key elements of the HealthCall system include an interactive dashboard, encounter management tools, evidence-based care plans, and HealthCall APR™. Interactive dashboards and encounter management tools give managers and clinicians access to real-time analytics that can improve decision-making. Evidence-based care plans are designed to engage the patient in self-care skills and behaviors, such as medication management, symptom management, and lifestyle modification. These case plans are highly configurable, allowing for a personalized, patient-centered experience. HealthCall APR™ provides a collection of device-enabled and patient-generated data from outside of the healthcare setting, providing greater insight and transparency by allowing clinicians to monitor each patient’s journey, intervening when necessary.
The Data:
Table 1. Readmission reduction percentage by program
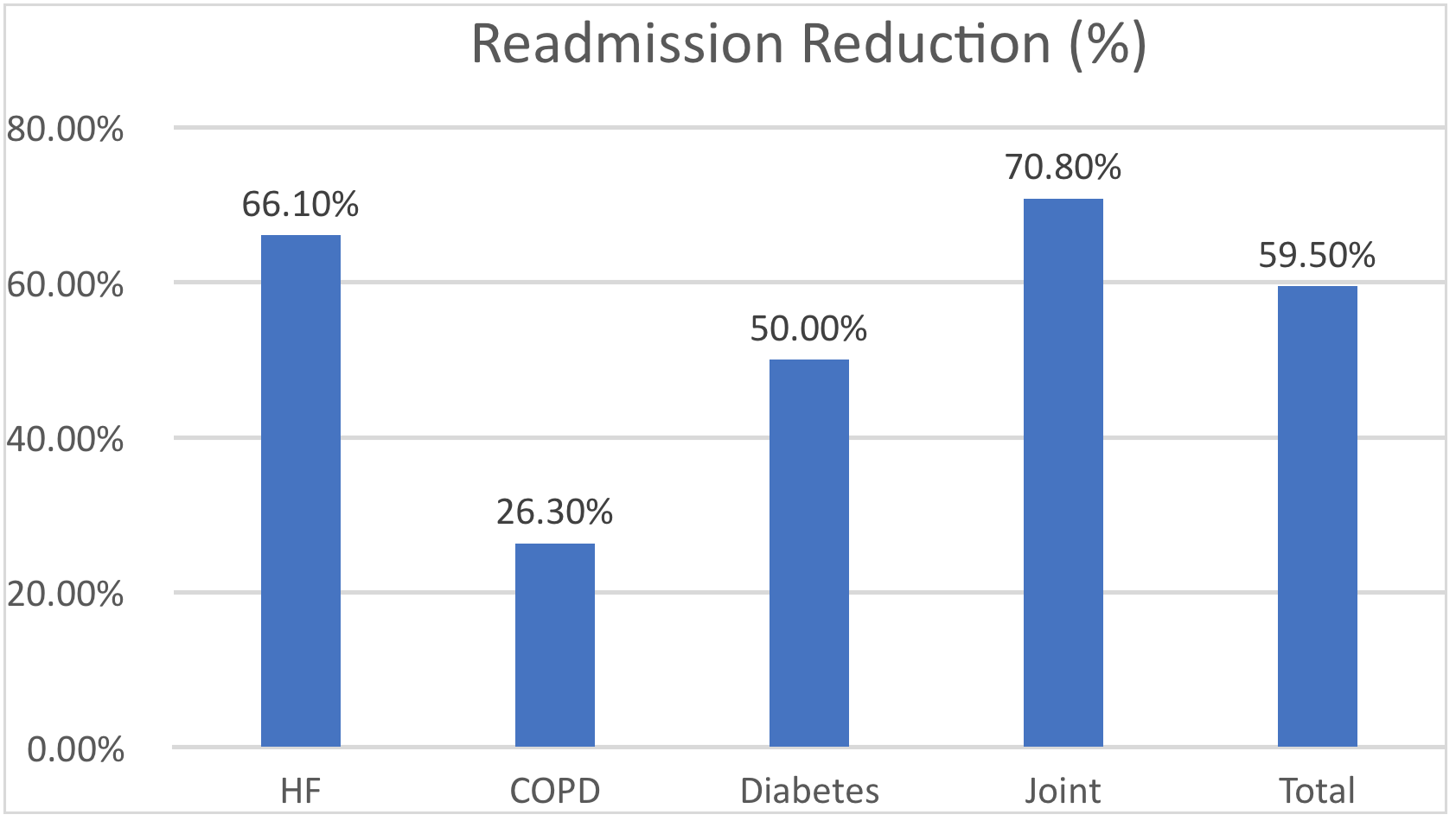
This case study included an analysis of hospital admissions/readmissions 180 days prior to the start date and 180 days after the start date. Patient populations included heart failure, COPD, diabetes, and joint replacement. The patient mix included 1,149 patients, including 212 heart failure patients, 69 COPD patients, 86 diabetic patients, and 782 joint replacement patients. The timeframe was from July 2016 through June 2017. The largest volume was in the Medicare population and 53.7% of the patients were over 65 years of age.
We noted a 59.5% reduction in admissions after the start date. This included a 66.1% reduction in heart failure, a 26.3% reduction in COPD, a 50% reduction in diabetes, and a 70.8% reduction in joint readmissions (Table 1).
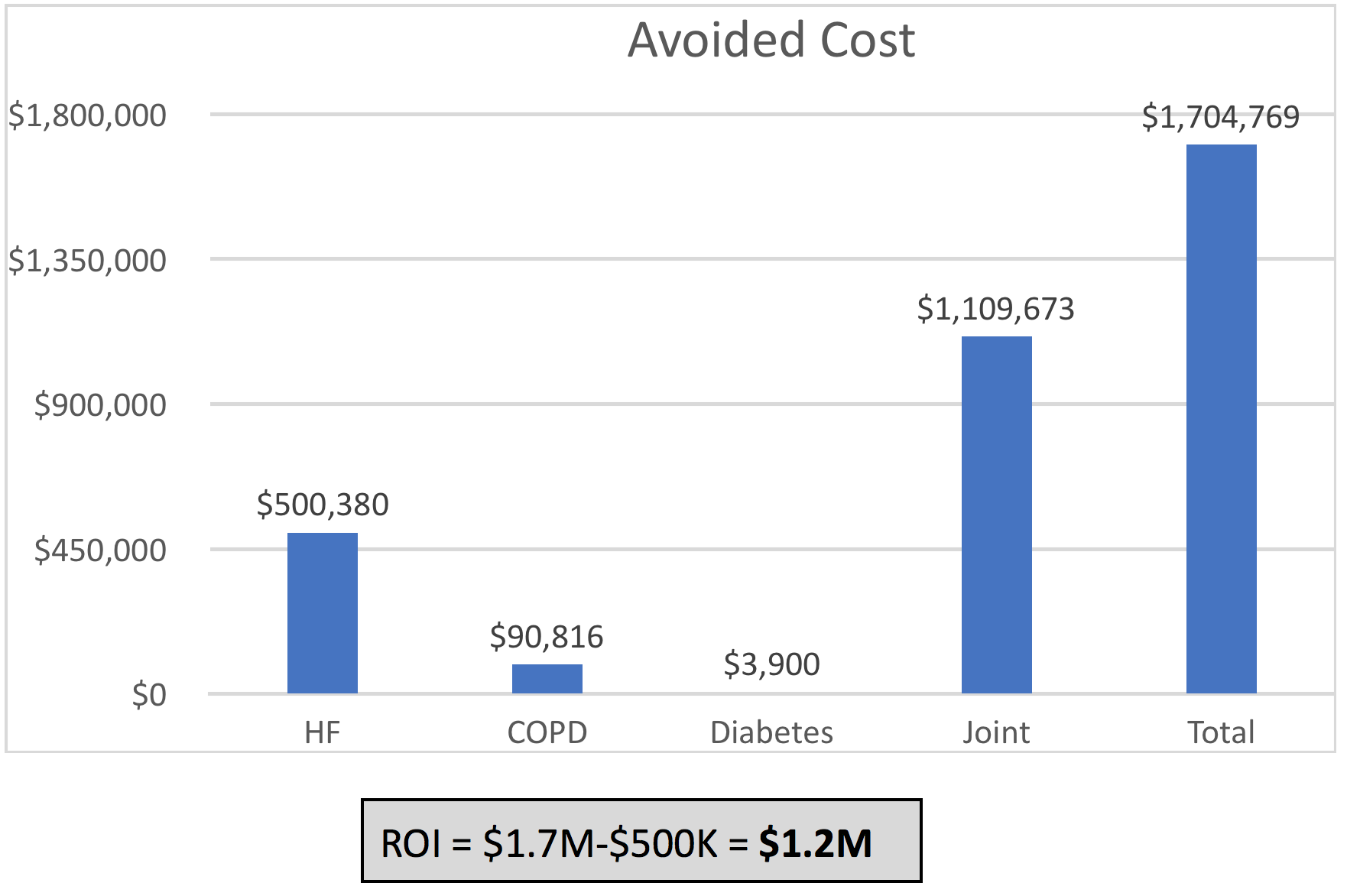
The reduction in readmissions resulted in significant cost savings, resulting in a total savings of $1.7 million and a cost of $500K. The return on investment, therefore, was estimated to be $1.2 million (Table 2). The program cost was based on a daily census of 300 patients and 4.8 full-time employees (FTEs).
Table 2. Avoided cost and return on investment by program
Analysis
The data from this case study indicates that readmissions can be reduced across multiple conditions pathways, resulting in a positive return on investment. While a cost savings of $1.2 million was achieved with an average of 300 patients in the program, even greater savings can be achieved at higher volumes.
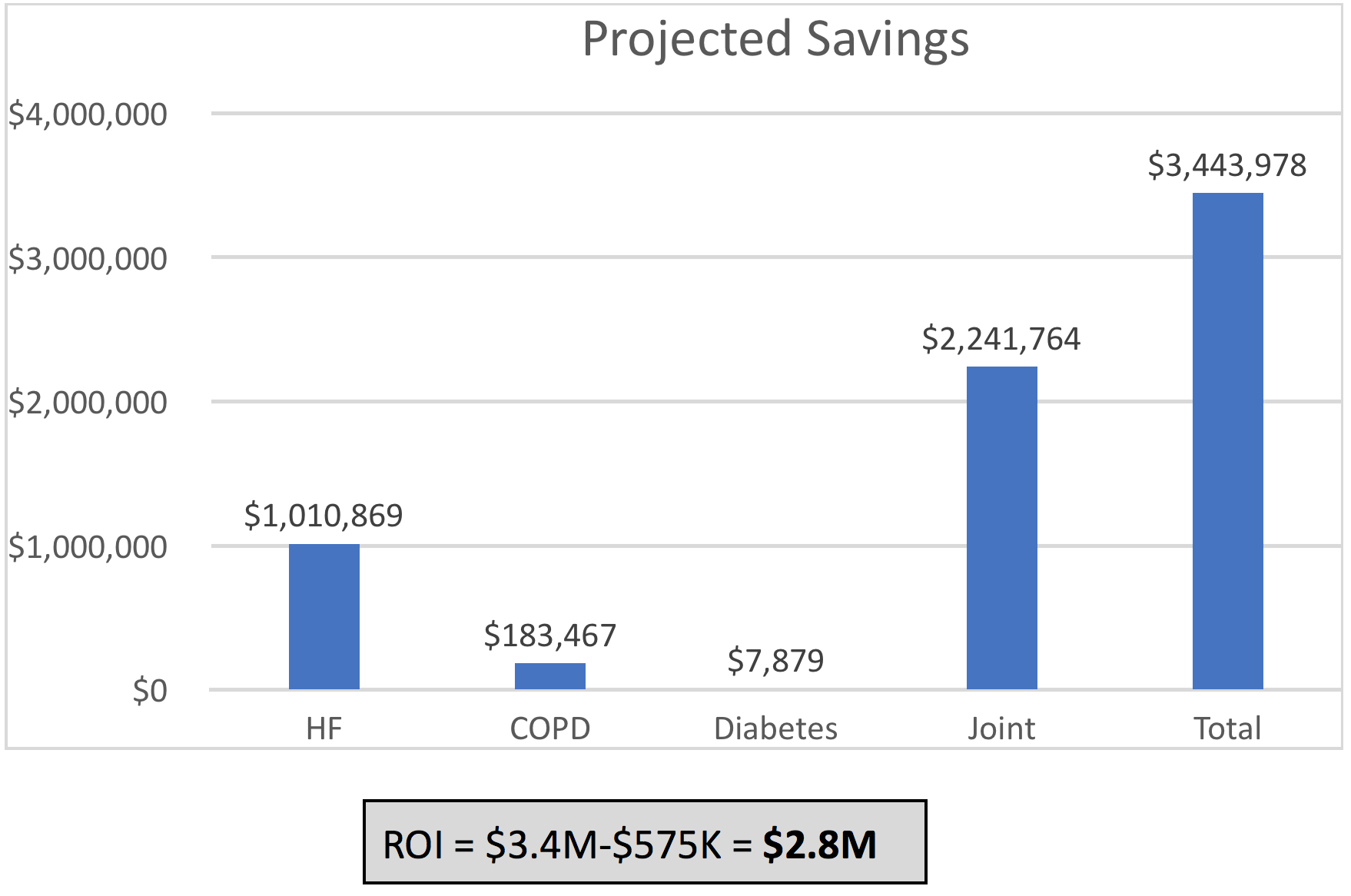
It is projected that when 2,000 patients are in the program the total savings will be $3,443,978 at a cost of $575K, resulting in a return on investment of $2,868,978 (Table 3).
The readmission reduction is highest in the heart failure and joint replacement programs. These programs also represent the largest patient populations, resulting in the higher ROI. However, all four of these patient populations require a high level of patient involvement, and even a single bad outcome can lead to significantly higher cost and greater impact on the lives of the patients and their families.
These results are not surprising, as HealthCall has consistently demonstrated significant reductions in readmissions resulting in cost savings and a positive return on investment. The HealthCall approach is extremely patient centric and does not attempt to restrict access to healthcare services.
Table 3. Projected savings with 2000 patients
Conclusion:
This case study demonstrates the cost-effectiveness of monitoring patients with chronic health conditions by reducing readmissions and improving the overall care of the patient. The HealthCall system uses state-of-the-art technology in the delivery of its program to these patients and their clinicians, and it does so in a patient-centered way, resulting in a better experience for both the patients and the healthcare team.
References:
1. Centers for Medicare and Medicaid Services. National Health Expenditures 2016 Highlights. Available online: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/highlights.pdf, last accessed June 10, 2018.
2. Buttorff C, Ruder T, Bauman M. Multiple Chronic Conditions in the United States Cdc-pdf[PDF – 392 KB]External. Santa Monica, CA: Rand Corp.; 2017.
3. Centers for Medicare and Medicaid. Hospital Readmission Reduction Program (HRRP). Retrieved from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html
4. Healthy People 2020. Factors that determine health status. Retrieved from: https://www.healthypeople.gov/2020/about/foundation-health-measures/Determinants-of-Health
5. Dunn, P & Conard, S. (2018). Improving health literacy in patients with chronic conditions: A call to action. International Journal of Cardiology. 273;249-251.
